1801006066 - LONG CASE
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 48 year Male patient came to the medicine OPD with chief complaints of
- Difficulty in breathing since 6 days
- decreased urinary output since 6 days
- Swelling of lower limbs on and off since 1 year
HISTORY OF PRESENTING ILLNESS
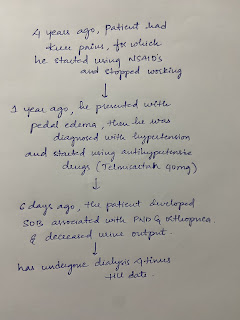
Patient was apparently asymptomatic 1 year back, then he developed bilateral pedal edema which is on and off in nature and pitting type since 1 year from knee to ankle region, and was on conservative treatment.
He went to local hospital and was diagnosed with hypertension and started using medication (drug-Telmisartan dosage-40mg)since 1 year.
6 days ago at night, the patient developed sob (grade 3) which is sudden in onset and gradually progressive, associated with orthopnea and pnd.
urine output is decreased - narrow streamlined urine.
no h/o cough
not associated with chest pain
not associated with sweating
no history of burning micturition
The patient has undergone dialysis 3 times since his admission.
DAILY ROUTINE
patient wakes up at 5:30am in the morning and does his household chores and goes to work daily work for 5 hours and comes back between 12-1 pm to have lunch, and takes rest for the day. Patient have dinner at around 7:30pm in evening and goes to sleep at 9pm.
PAST HISTORY
Known case of hypertension
No similar complaints in the past
Not a known case of DM, asthma, epilepsy, thyroid disorders.
DRUG HISTORY
Started using Telmisartan 40 mg since 1yr
FAMILY HISTORY
No similar complaints in the past
PERSONAL HISTORY
Appetite - Normal
Diet - mixed
Sleep - Adequate
Bowel and bladder - Regular but Decreased micturition
Addictions Smoking history -beedi consumer (4 beedis per day so 6 pack years)
Alcohol history -since 25 years 4 times monthly(whisky 90 ml each time)
GENERAL EXAMINATION
Patient is consious, coherent, and cooperative moderately built and moderately nourished.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Pedal edema - absent
VITALS:
Temperature - Afebrile
Pulse - 76 bpm
Blood pressure- 130/80 mmhg
Respiratory rate- 17 cycles per min
Spo2 - 95%
SYSTEMIC EXAMINATION
CVS:
Inspection:
No visible pulsations
Jvp is not raised
No precordial bulge
No chest wall defects.
Palpation:
Apex beat is at 6th intercoastal space in anterior axillary line.
No parasternal heave
No palpable P2
Auscultations:
S1 S2 heard
RESPIRATORY SYSTEM:
Inspection:
No scars, pulsation, engorged veins.
Ulcer present medial to right nipple
shape of chest - elliptical
chest is bilaterally symmetrical
bilateral airway entry present
trachea - Midline
Palpation:
Trachea is midline
Symmetrical chest expansion
Chest circumference is 34 inches
No tenderness.
Percussion-
right left
supra clavicular resonant resonant
infra clavicular resonant resonant
supra mammary resonant resonant
infra mammary resonant resonant
axillary resonant resonant
supra axillary resonant resonant
infra axillary resonant resonant
supra scapular resonant resonant
infra scapular resonant resonant
Auscultation- wheezing heard diffusely around chest
ABDOMINAL EXAMINATION:
shape- scaphoid
tenderness no
no palpable mass
liver not palpable
spleen not palpable
CNS EXAMINATION
speech normal
no focal neurological deficits seen
FINDINGS:
INVESTIGATIONS:
COMPLETE BLOOD PICTURE:
hemoglobin - 8.1gm/dl
total count - 12,680 cells/cumm
neutrophils - 74%
lymphocytes - 12%
pcv - 25.0%
blood group A+
interpretation- Normocytic normochromic anemia with neutrophilic leukocytosis
Platelet count - 2.16 lakhs/cu.mm
COMPLETE URINE EXAMINATION:
albumin ++
sugar nil
pus cells 2-3
epithelial cells 2-3
Red blood cells 4-5
random blood sugar - 124 mg/dl
RENAL FUNCTION TESTS:
urea 123 mg/dl
creatinine 5.7 mg/dl
uric acid 7.8 mg/dl
sodium 138 mEq/L
Potassium 3.3 mEq/L
Serum Iron- 74 ug/dl
24H URINE PROTEIN/ CREATININE RATIO:
Urine protein- 185 mg/dl
Urine creatinine - 0.5g/day
Ratio: 0.37
Urine volume- 125ml
LIVER FUNCTION TESTS:
Alkaline phosphate 312 mg/dl
total protein 6.2 gm/dl
albumin 3.04gm/dl
ABG ANALYSIS:
pH - 7.13
pCO2 - 34.6 mmHg
pO2 - 64 mmHg
HCO3 -21.1 mmol/L
O2 saturation 92.1%
X-ray CHEST:
- Ryles feed -100ml milk +protein powder 2 scoops
- Neb. Budecort and duolin 8hrly
- Inj. piptaz 2.25 gm iv-TID
- Inj.Lasix 40mg IV/BD
- Inj.Pan 40mg IV/OD
- Inj.Hydrocort 100 mg IV/BD
- Tab.Telma H
- Dialysis
- strict I/O charting
- Monitor vitals












Comments
Post a Comment